Pure HealthyBack and Blue Care Network of Michigan
Functional Restoration Clinical Outcomes Report July 13, 2015


Measurement Period: June 30, 2015
Report Delivery: July 13, 2015
Table of Contents
- Outcomes Overview
- Outcomes Measures
- Patient–‐reported Outcomes (PROs)
- Clinic–‐based Outcomes (CBOs)
- Outcomes Results: Patient Reported Outcomes (PRO)
- Pain
- Function
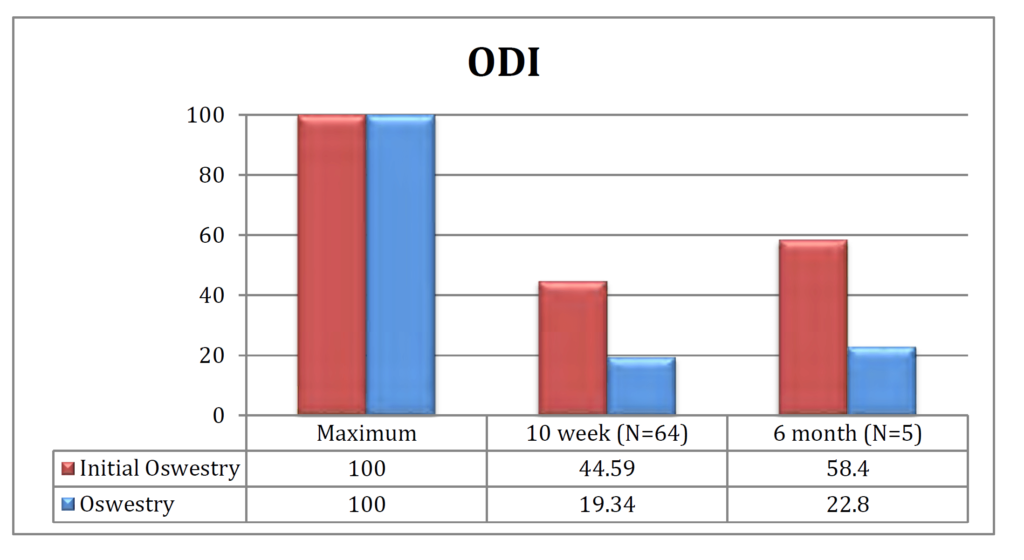
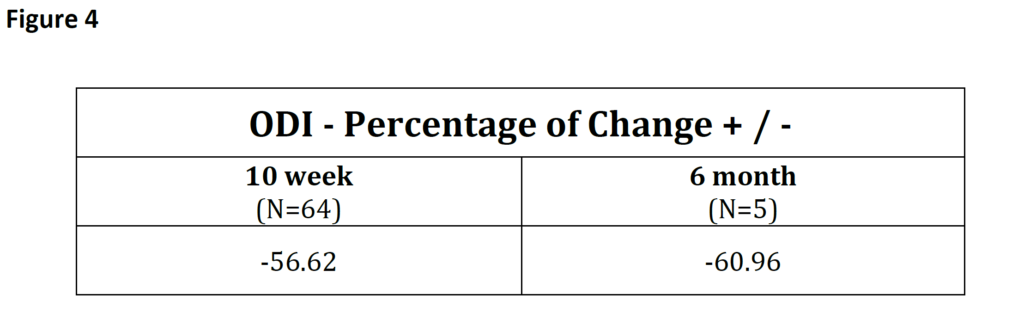
- Oswestry Disability Index (ODI)
- Patient Centered Outcome (PCO)
- Assessment of Quality of Life (AQoL)
- Outcomes Results: Clinical Based Outcomes (CBO)
- Lumbar and Cervical Strength/ROM
- Patient Satisfaction Scores
Outcomes Overview
The Pure HealthyBack (PHB) partnership with Blue Care Network of Michigan (BCNM) began to enroll patients in the third quarter 2014. Pure HealthyBack is the only company in the United States that provides evidence based, protocol driven spinal rehabilitation. In the era of the Patient Protection and Affordable Care Act, Accountable Care Organizations and the movement toward transparency, the PHB model leads the nation in metric based rehabilitation. As a result, the Blue Care Network of Michigan partnership with PHB is one of a distinctive group of programs that actively treats chronic neck and back pain patients and combines patient reported outcomes (PROs), clinician based outcomes (CBOs) and proactive healthcare coaching.
As of May 31, 2015, the Blue Care Network of Michigan program has 78 patients that have completed the 10- week program as well as 6 patients that are 6 months out. Blue Care Network of Michigan has exhibited significant clinical improvement as demonstrated by reduction in patient reported outcomes (PROs) of pain (- 52%) and disability (-55%), with increases in function (+250%), quality of life (+35%).
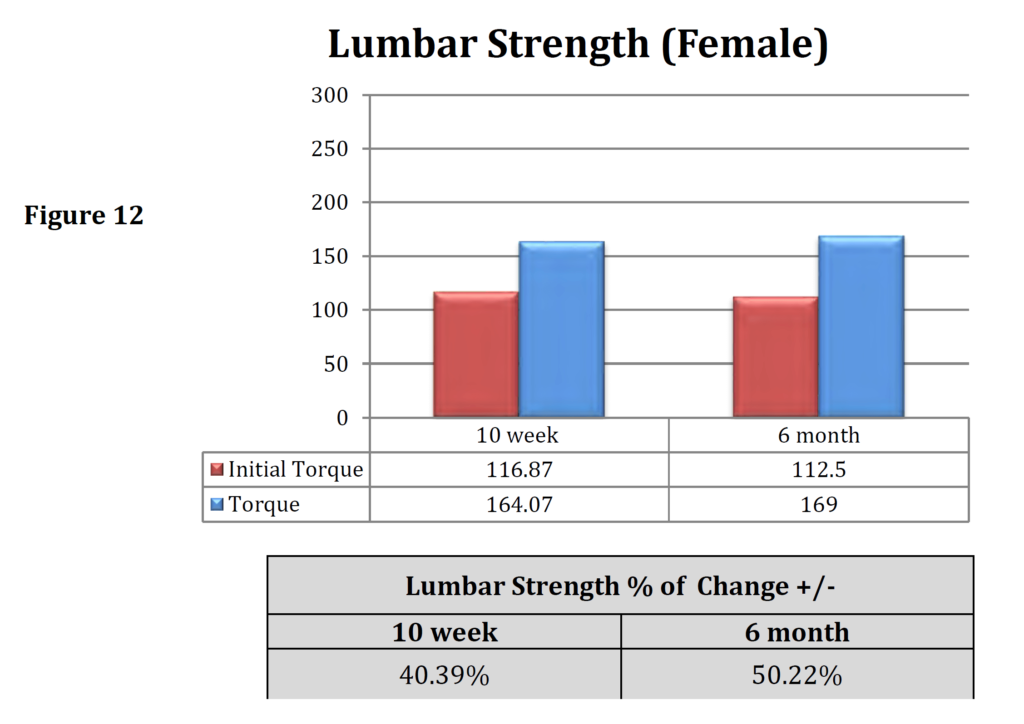
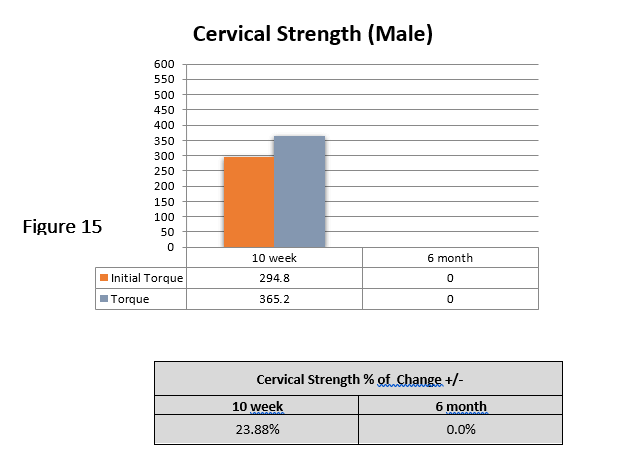
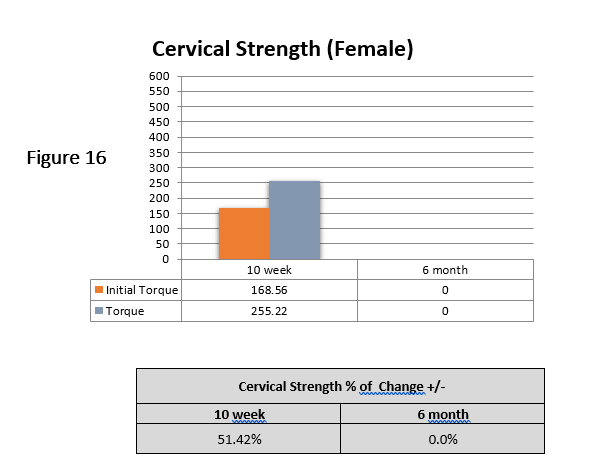
In addition, clinician based outcomes (CBOs) representing measured performance improvements in lumbar and cervical strength were +50% and +37% respectively.
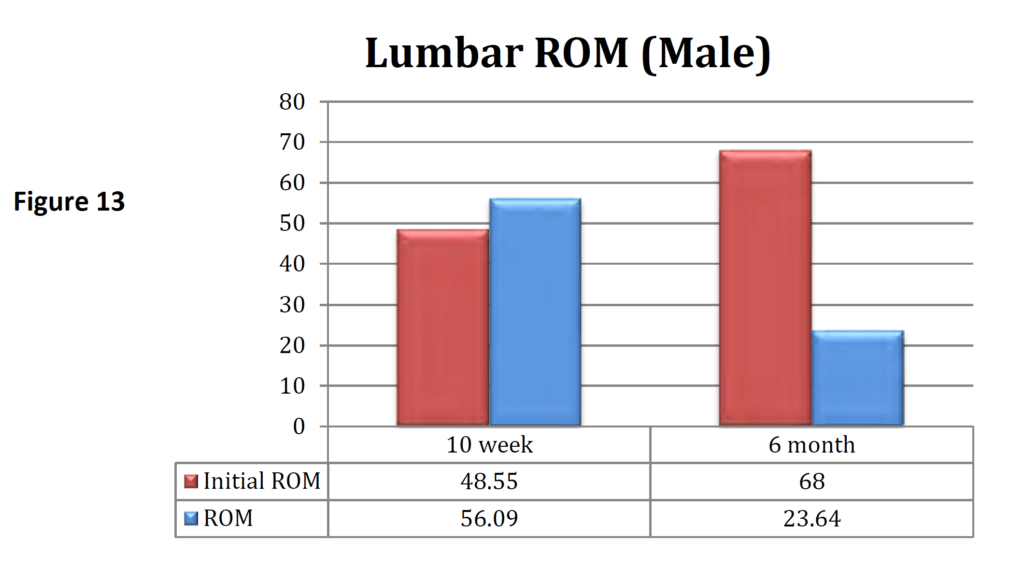
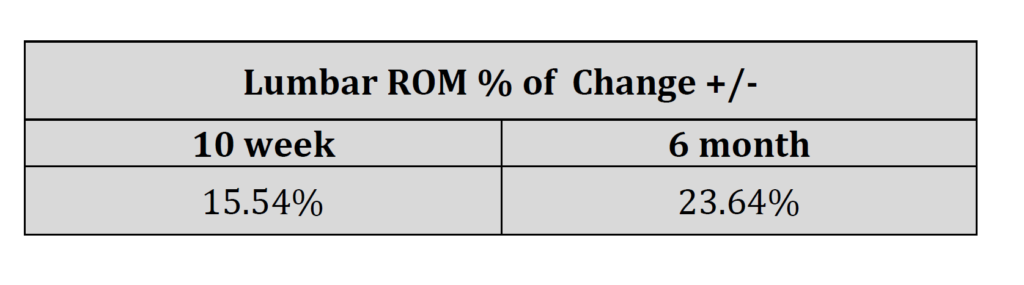
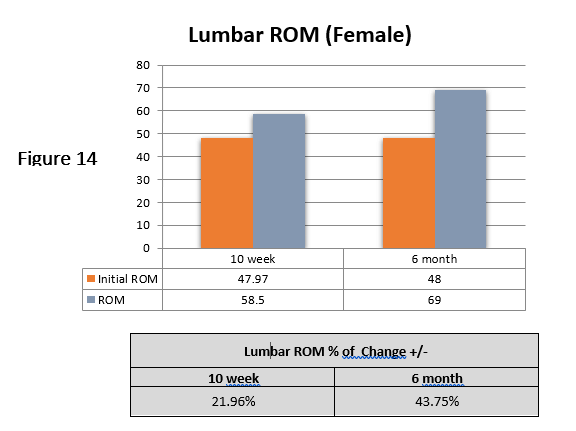
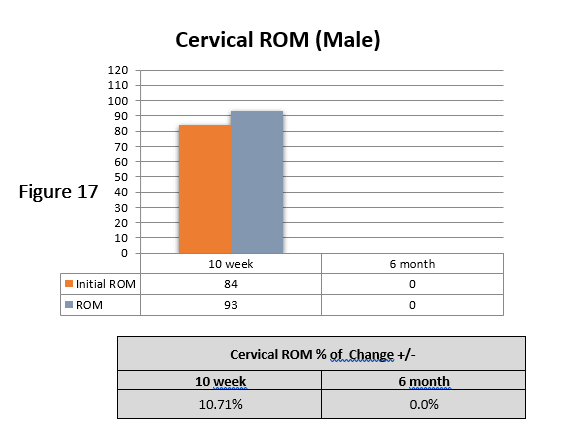
Improvements in Range of motion values (ROM) in lumbar and cervical were +26% and +37 % respectively.
These reported outcome measures demonstrate that the PHB program continues to be extremely successful in improving pain, disability, quality of life, patient satisfaction, strength and ROM for the patients in the Blue Care Network of Michigan.
Blue Care Network of Michigan is part of an elite group of clinics in the country at the forefront of accountable care because its comprehensive treatment approach for patients suffering from chronic back and neck pain, through its metric based evidence based rehabilitation model and demonstrated positive clinical results in both patient reported and clinic based outcomes.
Outcomes Measures
Patient-Reported Outcomes (PROs)
PROs are patient self-reports based on standardized questionnaires. These questionnaires ask each patient to rate their pain, their ability to perform certain functional tasks, and their quality of life.
Patient-reported Outcomes (PROs) include:
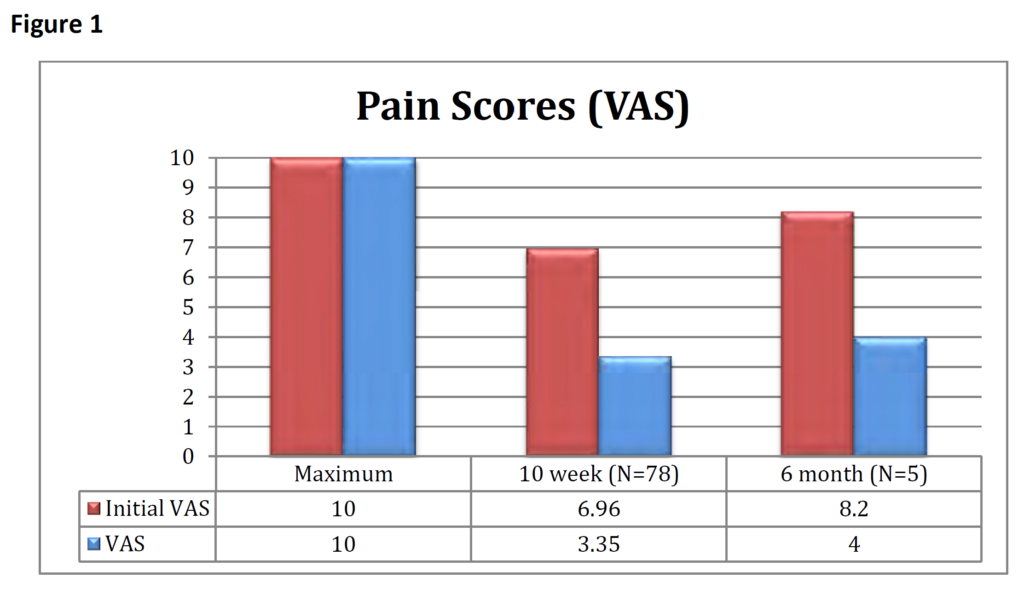
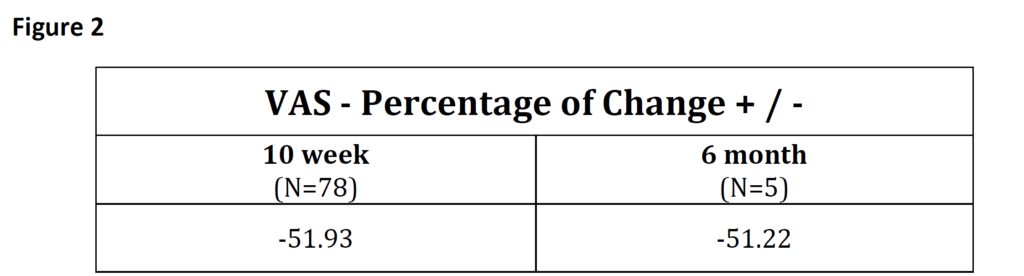
- Pain is measured using the Visual Analog Scale, which asks patients to rank their pain from 0 to 10 with 0 equaling no pain at all and 10 equaling the worst pain possible.
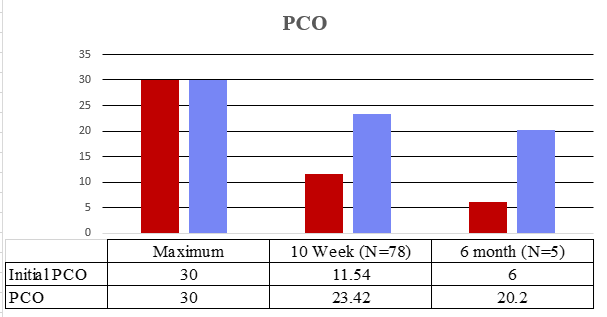
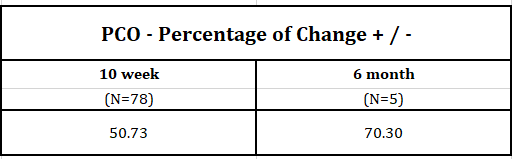
- Function is measured using the Patient-Centered Outcomes questionnaire, which asks patients to rank their abilities to function; 0 means that they are unable to function, and 30 is totally functional.
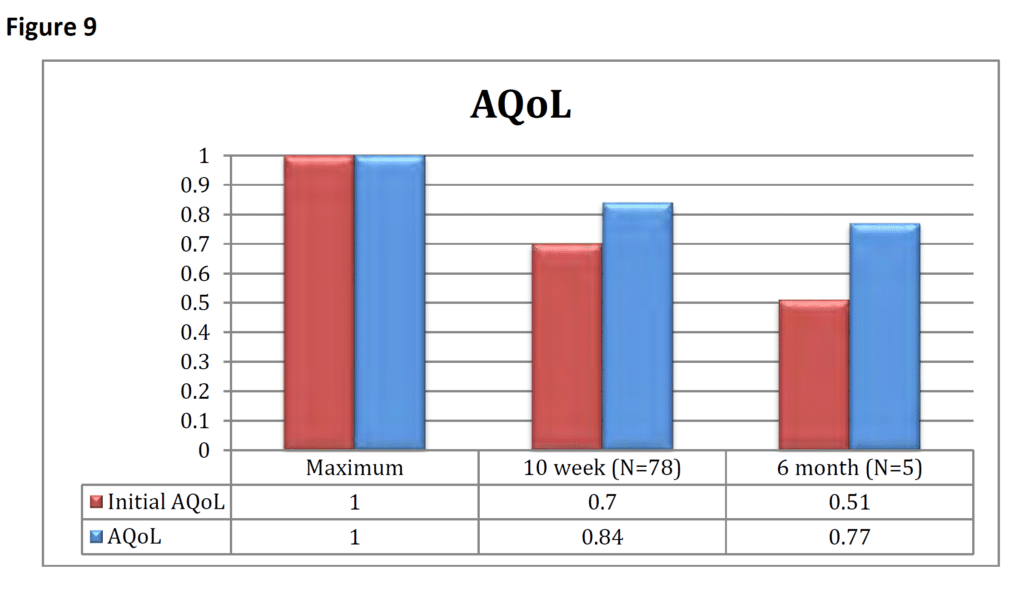
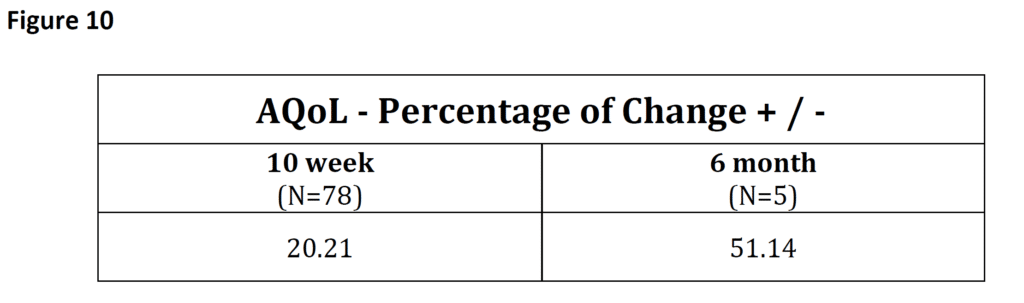
- Quality of Life is measured using the Assessment of Quality of Life questionnaire, which asks patients to rank their quality of life; 0 indicates no quality of life and 1.0 indicates the best quality of life.
Clinic-based Outcomes (CBOs)
Blue Care Network of Michigan CBOs are obtained by measuring patients’ lumbar or cervical range of motion and spinal strength on Pure HealthyBack’s FDA-registered proprietary medical equipment. Initial testing creates a baseline of patient performance and is used to develop individualized patient treatment prescriptions and to evaluate changes in the patient function as a result of the treatment program. Testing is safe, effective, and has been successfully utilized in thousands of chronic back/neck patients.
Over the last 25 years, the University of Florida, the University of California at San Diego, and medical institutions around the world have published compelling research showing exceptional results with specific spinal strengthening exercises using the PHB proprietary MedX lumbar and cervical extension machines. Over 75 peer-reviewed medical journal articles have been published affirming MedX’s ability to significantly decrease chronic spine-related pain issues, restore spinal function, improve quality of life and independence, and decrease or eliminate the need for ongoing spinal care or pain management.
Outcomes Results: Patient-reported Outcomes (PROs)
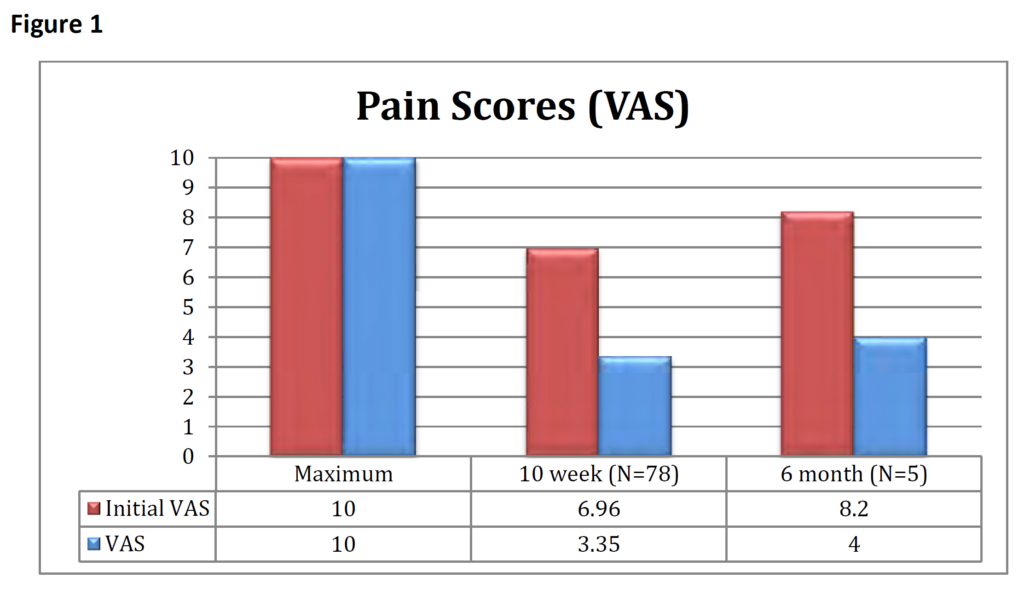
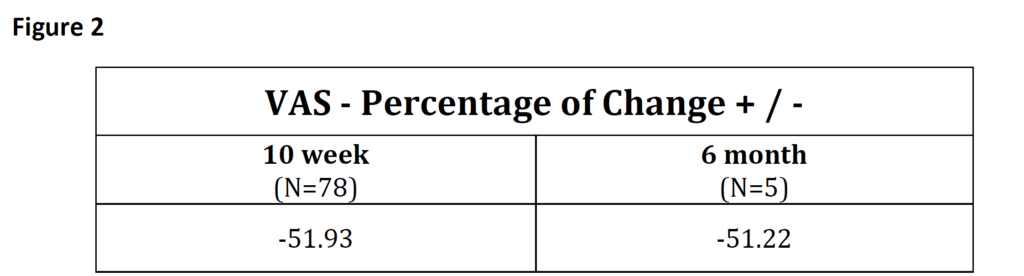
Pain: Patient pain is recorded using a Visual Analog Scale (VAS). Patients are asked before starting treatment to rate their pain from zero—meaning no pain—to 10, for the worst possible pain. Additional VAS scores are recorded after completing treatment and at successive milestone dates as indicted in Figure 1. The avg. overall significant reduction in pain of -51.58% (Figure 2) represents a drop from ‘intense’ to ‘mild’ pain.
Function: Indirect patient function is recorded in two ways through standardized functional questionnaires. Lumbar function is measured using the Oswestry Disability Index and cervical function is measured using the Neck Disability Index. Patient-generated functional goals are measured using the patient-centered outcomes
Neck Disability Index (NDI)
The NDI is the cervical counterpart of the ODI. It is a measure of each neck patient’s perceptions of their disability. The questionnaire asks 10 questions, each having six possible answers with a maximum disability score of 50 reflecting total disability. Topics include functional activities such as lifting, headache, concentration, and driving. Patients are given the NDI questionnaire and scored before starting treatment with additional scores recorded after completing treatment and at successive milestones dates as indicted in Figure 5. The avg. reduction in NDI scores of -53.14% (Figure 6) represents a significant drop in patients’ disability.
Patient Centered Outcomes (PCOs)
It is helpful for each patient to identify specific functional goals that are relevant in their personal lives with examples such as: gardening, lifting grandchildren, getting in and out of the car, and being more active in recreational activities. The PCO questionnaire asks each patient to list three items, each worth 10 points for a total of 30 points. They are asked to rank each item from 0—meaning they are unable to complete these activities—to 10, meaning they are completely able to complete these activities with no restrictions. Patients are given the PCO questionnaire and scored before starting treatment with additional scores recorded after completing treatment and at successive milestone dates as indicted in Figure 7. The avg. increase in PCO scores of +60.5% (Figure 8) represents a significant increase in patients’ function.
Assessment of Quality of Life (AQoL)
The AQoL is a standardized questionnaire that provides insight into each patient’s quality of life. In addition to reducing pain and increasing function, our goal is to enhance each patient’s life experiences. The AQoL asks about family/community relationships, sleep patterns, hearing, and sight, and has a maximum score of 1.0. Patients are given the AQoL questionnaire and scored before starting treatment with additional scores recorded after completing treatment and at successive milestone dates as indicted in Figure 9. The avg. increase in AQoL scores of 35.68% (Figure 10) represents a significant increase in patients’ quality of life.
Outcomes Results: Clinic-based Outcomes (CBOs)
Clinic-based Outcomes are founded on objective measurement of patients’ clinical performance and progress. Baseline measurements are taken of each patient’s lumbar and cervical strength and range of motion using proprietary technology that has been researched and published in medical journals over the past 25 years.
Initial testing provides measurements of the lumbar and/or cervical spine functional range of motion (ROM) by isolating the appropriate spinal segments to be treated. Once ROM is determined, strength of the lumbar and/or cervical extensors is measured as a baseline from which an individualized, clinical-strengthening prescription can be given to the patient. Knowing a patient’s initial capacity is critical to providing a program that is both safe and tailored specifically to the needs and limitations of each patient. Isometric testing has been performed on tens of thousands of patients and research documents measured positive changes for patients in strength gains, pain reduction, quality of life, and functional improvement. The following pages present Blue Care Network of Michigan clinical data on these variables in our patient populations.

Lumbar and Cervical Strength/ROM
The MedX lumbar and cervical patented technology provide objective measurement of spinal strength and range of motion. This data is presented in Figures 11 to 18 respectively along with percentage + /- changes.


Patient Satisfaction Scores
A major component in determining the overall quality and effectiveness of the program includes patient satisfaction survey results. Research has shown that patient satisfaction has a direct correlation to clinical outcomes and overall patient and program successes. We collect patient satisfaction data in four key areas that directly impact the total patient experience and to provide an overall assessment. Each area has a series of questions with a score of 1.0 indicating “Very Poor” to 5.0, indicating “Very Good”. The Blue Care Network of Michigan program rated on average above 4.7 in every category (as seen below), meaning the program has been rated as “Very Good” overall.
|
Physician Care Provider |
Score |
|
1. My appointments with my doctor were started on time. |
4.89 |
|
2. Ability to explain patient condition and answer questions. |
4.81 |
|
3. Interest in helping patient get better. |
4.96 |
|
4. Ability to make patient feel positive, supported, motivated. |
4.89 |
|
5. Patient trust in physician. |
4.89 |
|
6. Comprehensiveness of examinations. |
4.67 |
|
7. Longest amount of time (mins) kept waiting for doctor. |
2.80 |
|
Physician Care Provider Average |
4.85 |
|
Physical Therapy Providers |
Score |
|
1. My appointments with my therapist were started on time. |
4.89 |
|
2. Ability to make patient feel positive, supported, motivated. |
4.85 |
|
3. Ability to explain patient condition and answer questions. |
4.78 |
|
4. Interest in helping patient get better. |
4.93 |
|
5. Communication skills of your therapist. |
4.81 |
|
6. Attention provided to patient during visits. |
4.96 |
|
7. Patient trust in physical therapist. |
4.96 |
|
8. Longest amount of time (mins) kept waiting for therapist. |
2.54 |
|
Physical Therapy Provider Average |
4.88 |
|
Clinic Operations |
Score |
|
1. Hours of operation. |
4.70 |
|
2. Ease of accessing the clinic. |
4.33 |
|
3. Ability to maintain your privacy. |
4.89 |
|
4. Service provided to you by the front desk. |
4.89 |
|
5. Accuracy of scheduled appointments. |
4.78 |
|
6. Appointment reminder phone calls. |
4.78 |
|
7. Ease of scheduling appointments. |
4.78 |
|
8. Courtesy of people scheduling your appointment. |
4.89 |
|
9. Helpfulness on the telephone. |
4.89 |
|
10. Promptness in returning patient phone calls. |
4.85 |
|
11. Patient’s ability to schedule desired appointment time. |
4.67 |
|
Clinic Operations Average |
4.77 |
|
Wellness Trainer |
Score |
|
1. My wellness appointments started on time. |
4.81 |
|
2. Ability to make patient feel positive, supported, motivated. |
4.88 |
|
3. Ability to explain patient condition and answer questions. |
4.81 |
|
4. Interest in helping patient get better. |
4.94 |
|
5. Communication skills of your wellness trainer. |
4.94 |
|
6. Attention provided to patient during visits. |
4.94 |
|
7. Patient trust in wellness trainers. |
4.88 |
|
8. Longest amount of time kept waiting to start appointment. |
3.43 |
|
Wellness Trainer Average |
4.88 |
|
Overall Assessment |
Score |
|
1. Overall, how would patient rate quality of care in program. |
4.93 |
|
2. What is the likelihood you will recommend us to others. |
4.93 |
|
3. How would you rate the cleanliness of the clinic. |
4.96 |
|
Overall Assessment Average |
4.94 |
Conclusion
Blue Care Network of Michigan is deeply invested in the collection and use of clinic-based and patient-reported outcomes so that we can follow patient results both individually and as a population. We use this information to continuously refine what is already a leading-edge treatment model. As this report demonstrates, we continue to see significant improvements among our patients with reductions in pain and disability; increases in function and quality of life; outstanding improvements in lumbar and cervical strength and range of motion; and excellent patient satisfaction scores.